40 YEAR MALE WITH PAIN AND DISTENSION OF ABDOMEN , DECREASED URINE OUTPUT SINCE 2 DAYS
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
• A 40 year old male pt , farmer by occupation resident of Nalgonda came with
Chief complaints
Pain abdomen 2 days
Vomitings 1 day
Decreased urine output 1 day
No urine output 8hrs
History of present illness
Patient was apparently asymptomatic when he was 7 years old with a swelling on the midline lower lumbar region 2x2 cm on midline spine .
Since then patient complaining of involuntary urination frequently .
Patient used to use intermittent urinary catheter frequently to drain urine by himself
Patient was asymptomatic in between, on 30/10/2023 patient had complaints on pain abdomen ( epigastric ) which was insidious onset not radiating gradually proggresing aggrevating on food intake and relieved temporarily on medication .
3/12/2023
Patient complaining of pain abdomen in epigastric and umbulicus region , dragging type sudden onset gradually proggresive aggrevating on food intake and relieved temporarily on medications
• History of vomiting 1 episode non bilious non projectile not blood tinged not foul smelling food particals as content .
• Decreased urine output since 1 day
• No urine output since 8hrs
• patient also complaining of Shortness of breath since 1 day
Past history
Patient had a swelling of 2x2 cms on midline lower lumbar region for which he underwent surgery .
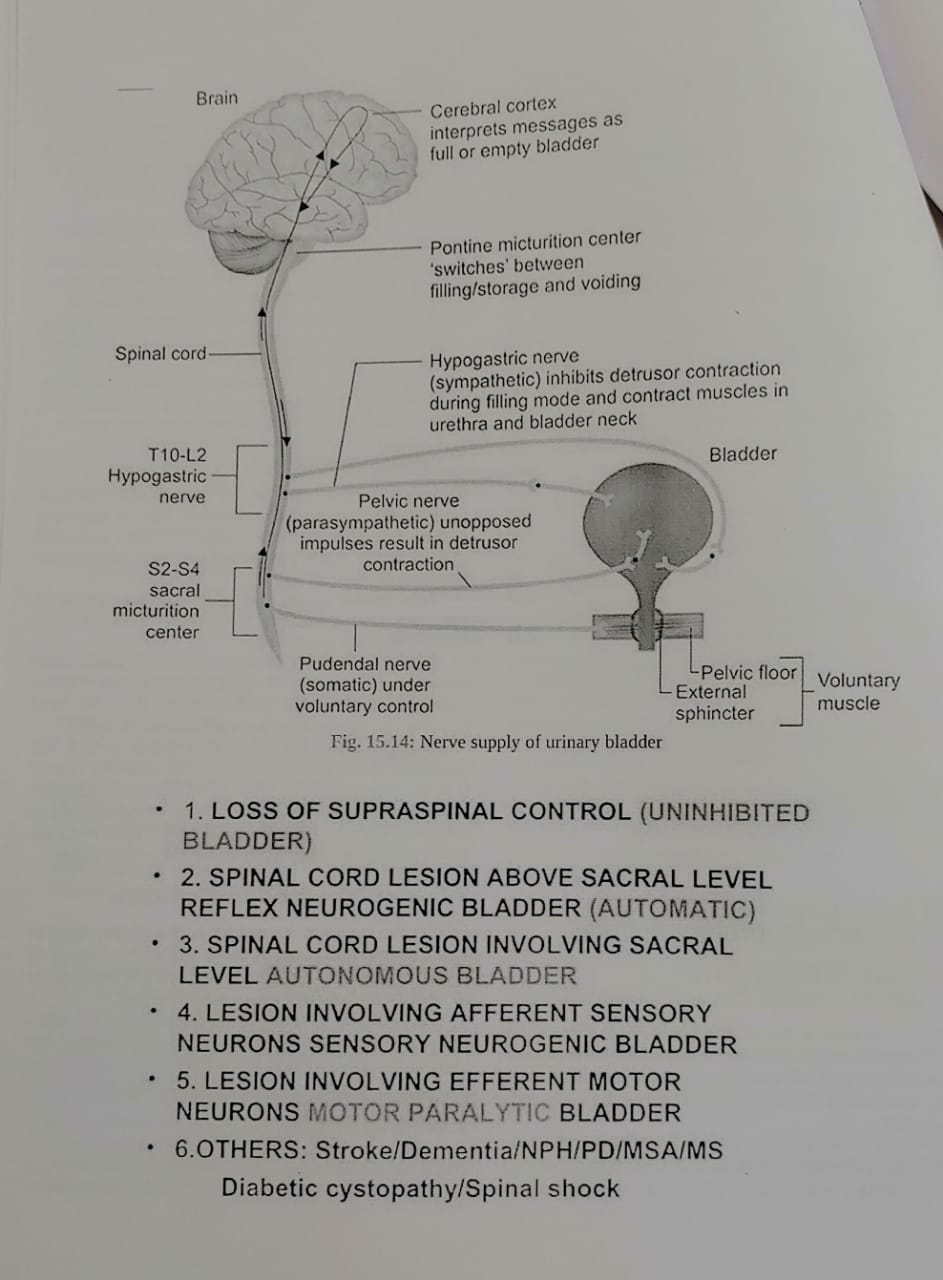
Since then he had neurogenic bladder and he is having involuntary dribbling of urine for ehich it is managed conservatively
• H/o Hypertension since 1 year
Family history
No significant family history
Drug History
Not on any hypertensive medication.
Personal history
Diet : mixed
Appetite: decreased
Sleep: decreased
Bowel and bladder movements : irregular (neurogenic bladder).
CARDIOVASCULAR SYSTEM
INSPECTION
Chest is elliptical shaped, bilaterally symmetrical.
Trachea appears to be central
Movements are equal bilaterally
JVP:Raised
No Visible epigastric pulsations
No scars or sinuses
PALPATION
All the inspectory findings are confirmed
Trachea is central
Apical impulse felt at 5th intercostal space lateral to midclavicular line.
AUSCULTATION
S1 S2 heard no murmurs
RESPIRATORY SYSTEM
INSPECTION
Chest is elliptical shaped,
bilateral symmetrical.
Trachea is central
Movements are equal bilaterally
No Visible epigastric pulsations
No scars or sinuses
Apical impulse not seen
PALPATION
All inspectory findings are confirmed: Trachea is central, movements equal bilaterally.
Antero-posterior diameter of chest >Transverse diameter of chest
Apex beat felt in 6th intercostal space lateral to midclavicular line
PERCUSSION
Resonant note heard in all areas bilaterally
AUSCULTATION
Bilateral air entry present – Normal vesicular breath sounds heard
PER ABDOMEN
INSPECTION
Shape of abdomen appears to normal
No Visible epigastric palpations
No engorged veins sinus scars
PALPATION
All inspectory findings conformed
Tenderness +
No organomegaly
PERCUSSION
Tympanic note heard all quadrants abdomen
AUSCULTATION
Bowel sounds heard in RIF
CENTRAL NERVOUS SYSTEM
Pt is C/C/C
HMF - Intact
Speech & language – Normal
Memory can recall
No Signs of Meningeal irritation
Motor and sensory system – Normal
Reflexes – Normal
Cranial Nerves – Intact
Gait – Normal
Cerebellum – Normal
GCS Score – 15/15
CRANIAL NERVE
OLFACTORY - NORMAL (SMELL)
OPTIC - Normal
OCCULOMOTOR - Normal
TROCHLEAR Normal
TRIGEMINAL Normal
ABDUCENS Normal
FACIAL NERVE Normal
VESTIBULOCOCHLEAR Normal
GLOSSOPHARYNGEAL Normal
VAGUS - Gag reflex present
SPINAL ACCESSORY Normal shrugging shoulders
HYPOGLOSSAL Normal ( Not deviated )
MOTOR SYSTEM
Bulk - MUSCLE WASTING IN LL > UL
Right. Left
Tone UL 2+ 2+
LL. 2+ 2+
Power. UL 2+ 2+
LL 2+ 2+
REFLEXES
Corneal - N
Conjuctival - N
Pharyngeal - N
Palatal -N
Abdominal -N
Cremasteric - N
DEEP TENDON REFLEX
Jaw Jerk - N
Biceps - N
Triceps - N
Supinator - N
Knee jerk - N
Ankle jerk- N
Clonus - absent
Position sense:
Right Left
Upper Limb N N
Lower Limb N N
-Graphaesthesia-Postive
-Stereognosis-Positive
Cerebellar signs:
-Titubation:absent
-Nystagmus:absent
-Dysarthria:absent
-Hypotonia:absent
-Intention tremor:absent
-Coordination
a.Finger Nose test: Normal
b.Heel Knee test: Normal
c. Dysdiadokokinesia: Negative( able to perform rapid alternative movements)
Signs of Meningeal Irritation:
Neck stiffness: absent
Kernig’s sign :absent
Brudzinski’s sign:absent
Clinical Images
6/12/2023
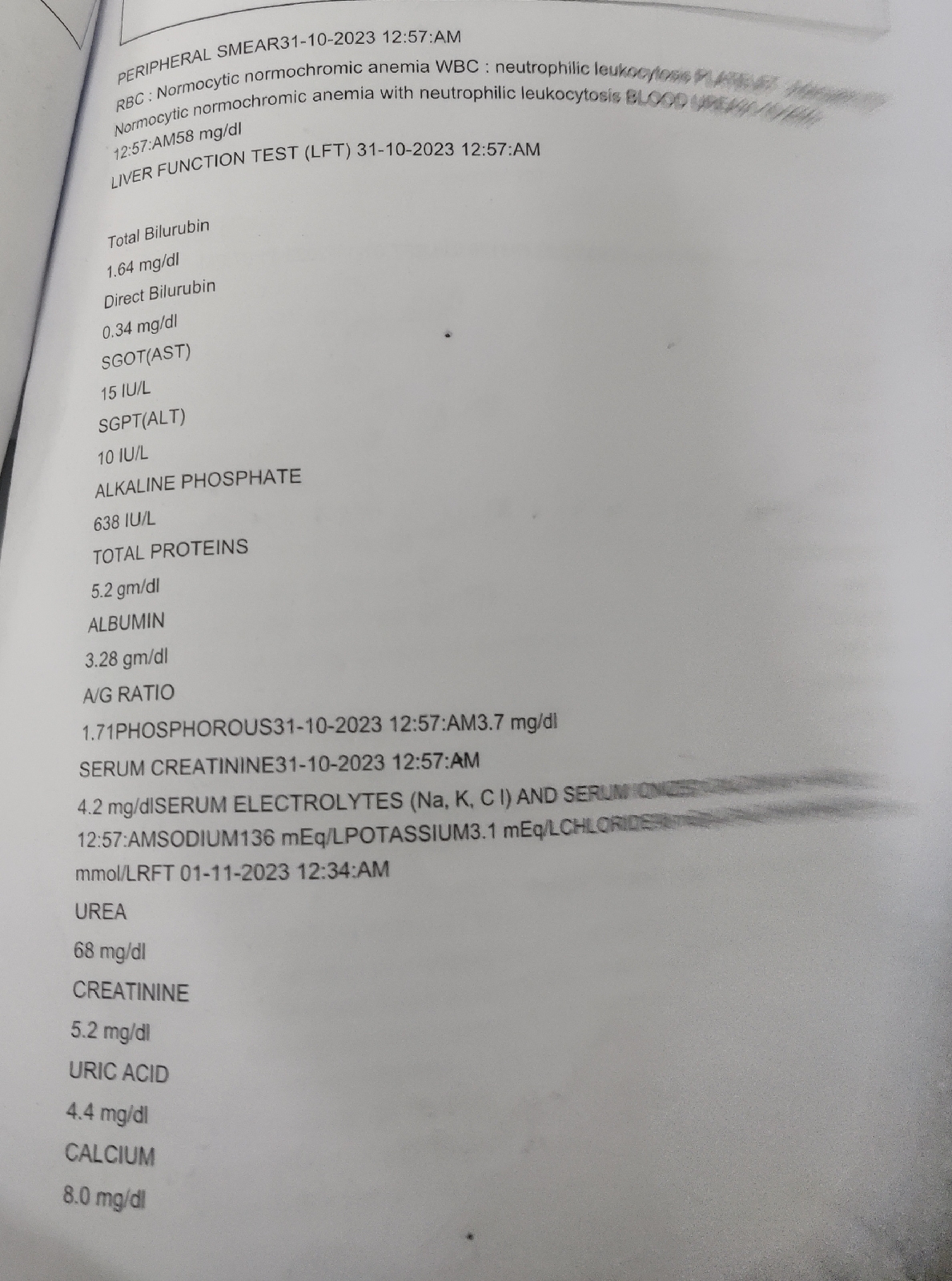
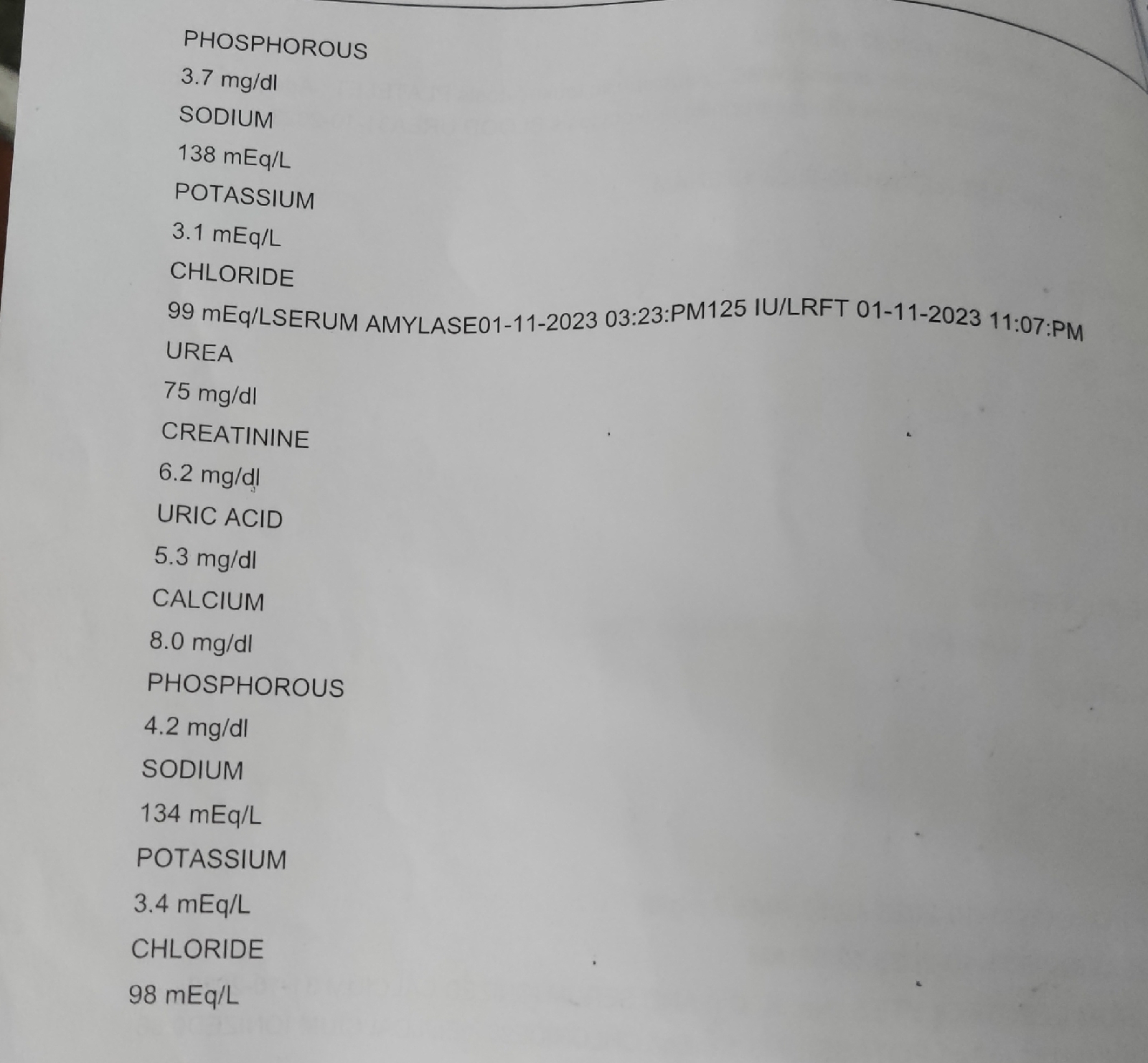
Investigations
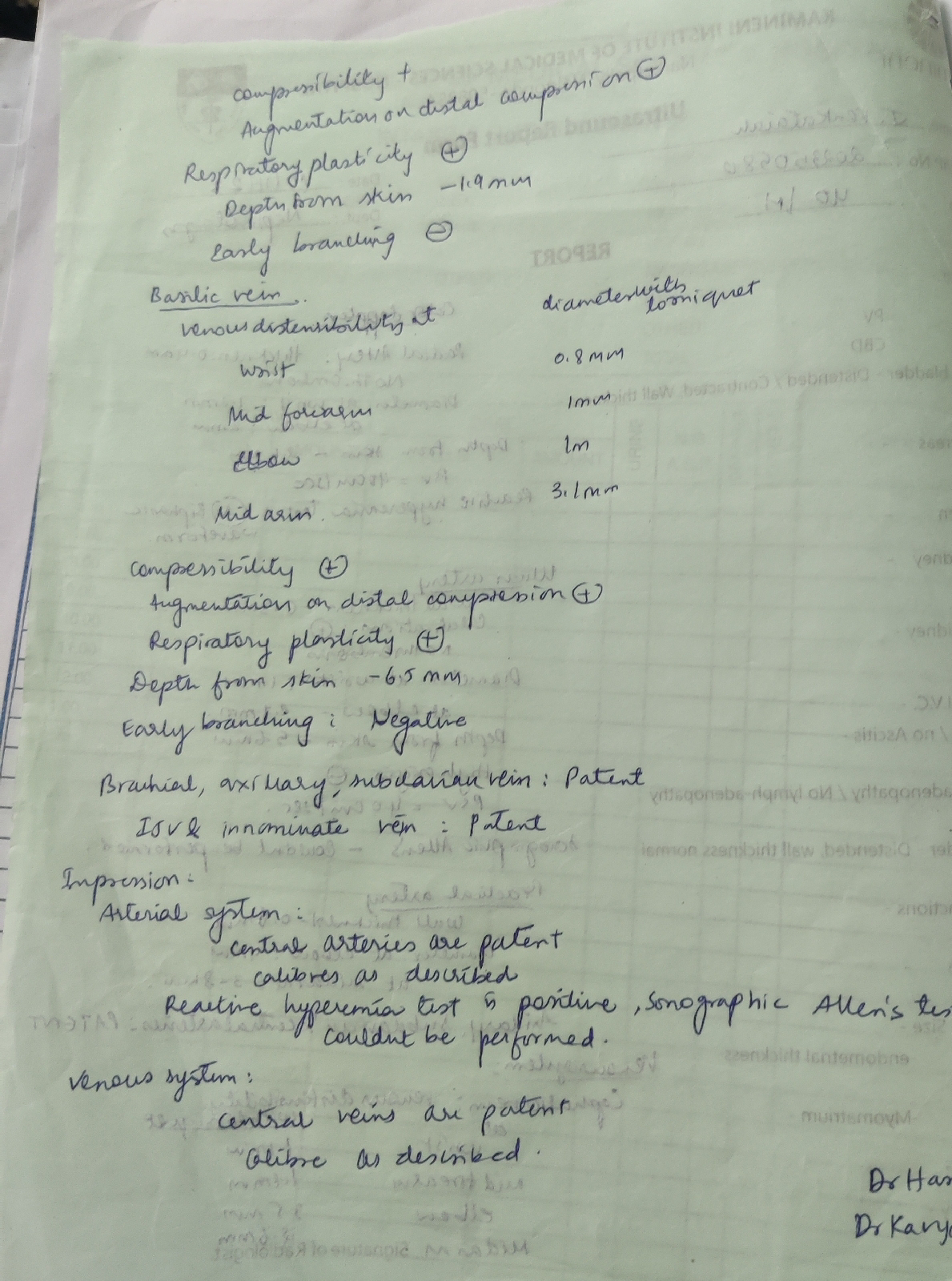
Ultrasound
Provisional Diagnosis
? High output heart failure
? Anemia of chronic disease
? AKI CKD
? Cauda equina syndrome
? pancreatitis
? Peritonitis
Treatment
Fluid restriction < 1.2 L/day
Salt restriction < 2g/day
T Lasix 40 mg po/BD
T Shelcal CT po/OD
T Nodosis 1 g po/OD
T Orofer XT PO /OD
T . Aricamin 0.1mg PO/TID
T. Minipres 2.5 mg PO/OD
T Senelemas 400 mg PO/BD
T. Pantoprozole 40 mg PO/OD
T.Nifidepine 20 mg PO/TID
T . Levocetrizine 5 mg PO/BD
Monitor vitals














Comments
Post a Comment