OSCE & LEARNING POINTS
OSCE
• Which is the better afterload reducing drug?
One of the classes of drugs commonly used to reduce afterload is vasodilators. Afterload refers to the resistance the heart has to overcome to eject blood into the systemic circulation. Vasodilators help dilate blood vessels, reducing this resistance and making it easier for the heart to pump blood. Several types of vasodilators are used for this purpose:
1. **Angiotensin-Converting Enzyme (ACE) Inhibitors:**
- **Examples:** Enalapril, Lisinopril, Ramipril.
- **Mechanism:** Inhibit the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor. This leads to vasodilation and reduced afterload.
2. **Angiotensin II Receptor Blockers (ARBs):**
- **Examples:** Losartan, Valsartan, Irbesartan.
- **Mechanism:** Block the action of angiotensin II on its receptors, resulting in vasodilation and decreased afterload.
3. **Calcium Channel Blockers:**
- **Examples:** Amlodipine, Nifedipine, Diltiazem.
- **Mechanism:** Inhibit the influx of calcium into vascular smooth muscle cells, leading to vasodilation and reduced afterload.
4. **Hydralazine:**
- **Mechanism:** Direct arterial vasodilation by affecting vascular smooth muscle.
- **Clinical Use:** Often used in combination with a nitrate for the treatment of heart failure.
5. **Nitrates:**
- **Examples:** Nitroglycerin, Isosorbide dinitrate.
- **Mechanism:** Release nitric oxide, leading to vasodilation, particularly in veins. This reduces preload and can also have an afterload-reducing effect.
The choice of the specific drug or combination of drugs depends on the patient's condition, the underlying cause of increased afterload, and individual response to the medications. These medications are commonly used in conditions like hypertension, heart failure, and certain forms of ischemic heart disease to improve cardiac function by reducing the workload on the heart. Always consult with a healthcare professional for personalized advice and prescription based on individual health circumstances.
• Cauda equina syndrome ?
The cauda equina is a bundle of spinal nerve roots located at the lower end of the spinal cord within the vertebral canal. The term "cauda equina" is Latin for "horse's tail," describing the nerve roots that extend beyond the spinal cord resembling a tail. Here are key points about the cauda equina:
1. **Location:** The cauda equina is situated in the lumbar (lower back) and sacral (pelvic) region of the spinal canal.
2. **Components:** It is composed of multiple nerve roots that emerge from the end of the spinal cord. These nerve roots continue down the vertebral canal before branching out to various structures in the lower part of the body.
3. **Function:** The cauda equina is responsible for transmitting nerve signals to and from the pelvic organs, lower limbs, and perineum. It plays a crucial role in motor and sensory functions.
4. **Clinical Significance:**
- **Cauda Equina Syndrome (CES):** This is a rare but serious condition where the nerve roots of the cauda equina are compressed. CES can result from conditions such as a herniated disc, tumor, infection, or trauma. Symptoms may include severe lower back pain, bilateral leg weakness, numbness in the saddle area, and loss of bladder or bowel control. CES is considered a medical emergency requiring immediate attention and intervention.
5. **Diagnosis:**
- **Clinical Evaluation:** A thorough clinical examination, including assessing sensory and motor function, reflexes, and bladder and bowel function.
- **Imaging Studies:** Magnetic Resonance Imaging (MRI) is often used to visualize the spinal cord and nerve roots, helping identify the cause of compression.
6. **Treatment:**
- **Surgical Intervention:** In cases of Cauda Equina Syndrome due to compression, prompt surgical decompression is typically necessary to relieve pressure on the nerve roots.
- **Medication:** Depending on the underlying cause, medications may be prescribed to manage pain, inflammation, or infections.
Cauda equina plays a vital role in the communication between the spinal cord and the lower part of the body. Conditions affecting this region, particularly Cauda Equina Syndrome, require urgent medical attention to prevent irreversible damage and address the underlying cause. Individuals experiencing symptoms suggestive of CES should seek immediate medical care.
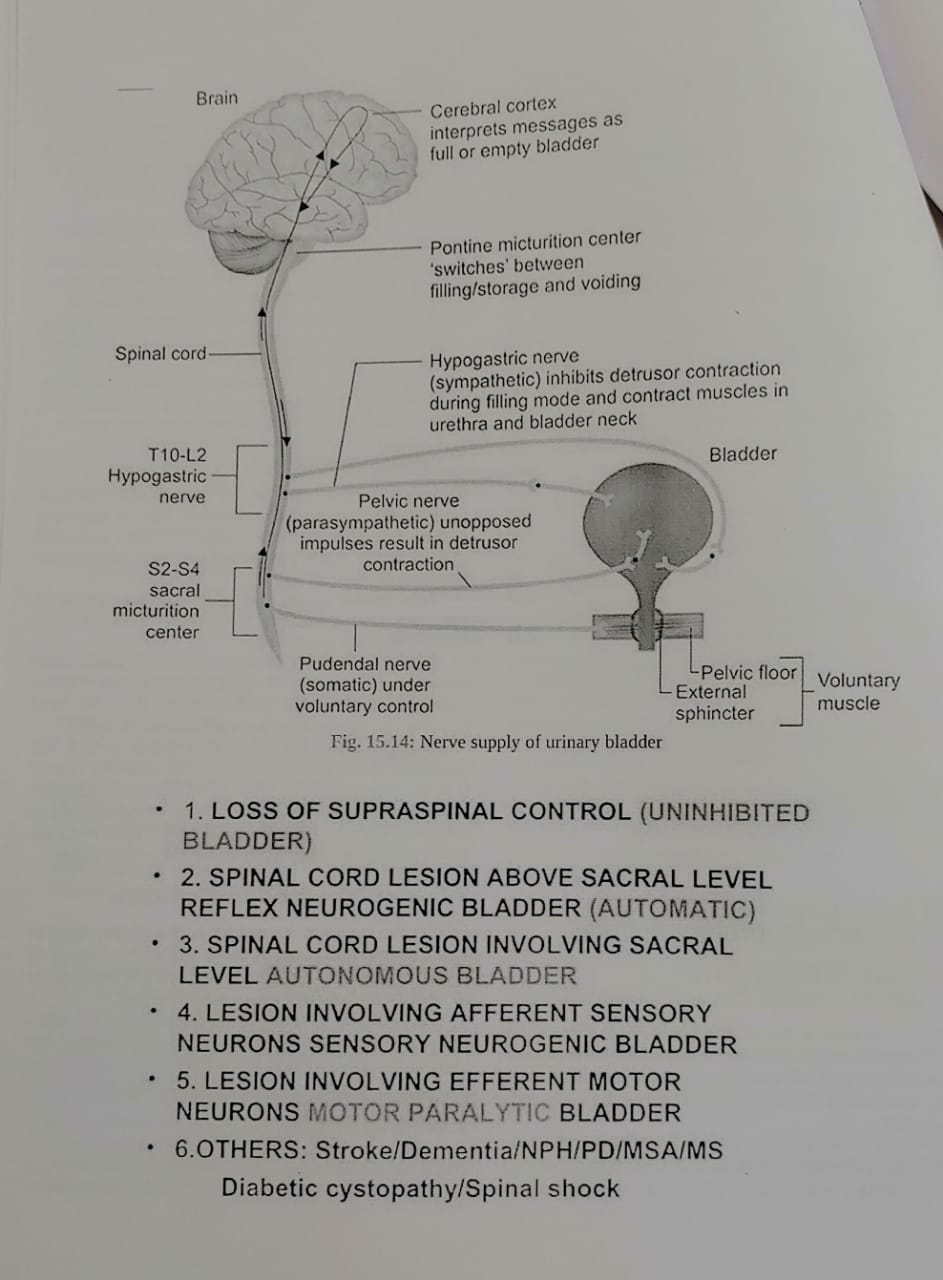
• Neurogenic bladder ?
Neurogenic bladder refers to a dysfunction of the urinary bladder due to a neurological problem, which disrupts the normal nerve signals between the bladder and the brain. This condition can affect the storage and release of urine, leading to various symptoms. Here are key points about neurogenic bladder:
1. **Causes:** Neurogenic bladder can result from a variety of neurological conditions or injuries, including spinal cord injuries, multiple sclerosis, Parkinson's disease, stroke, spinal cord tumors, or nerve damage related to diabetes.
2. **Symptoms:**
- **Urinary Incontinence:** Loss of bladder control, which may lead to leakage of urine.
- **Urinary Retention:** Inability to empty the bladder completely.
- **Frequency and Urgency:** Frequent or urgent need to urinate.
- **Nocturia:** Increased need to urinate during the night.
- **Incomplete Emptying:** Difficulty fully emptying the bladder.
3. **Types:**
- **Overactive Bladder (OAB):** Characterized by urgency, frequency, and sometimes urge incontinence.
- **Underactive Bladder:** Results in difficulty initiating or completing urination.
4. **Diagnosis:** A healthcare provider may use various tests, such as urodynamic studies, cystoscopy, and imaging studies, to assess bladder function and identify the underlying neurological cause.
5. **Treatment:**
- **Medications:** Depending on the type of neurogenic bladder, medications may be prescribed to relax the bladder muscles (antimuscarinics) or stimulate bladder contractions (cholinergics).
- **Catheterization:** Intermittent self-catheterization or the use of an indwelling catheter may be necessary to empty the bladder.
• Paraparesis ?
Paraparesis refers to a condition characterized by weakness or partial paralysis affecting the lower limbs, typically involving both legs. It is a subset of the broader term "paresis," which refers to muscle weakness or partial loss of movement.
- key points about paraparesis:
1. **Bilateral Leg Involvement:** Paraparesis specifically involves weakness or impaired function in both legs.
2. **Causes:**
- **Spinal Cord Disorders:** Conditions affecting the spinal cord, such as spinal cord injuries, spinal cord tumors, or degenerative spinal disorders, can lead to paraparesis.
- **Neurological Disorders:** Certain neurological conditions like multiple sclerosis or transverse myelitis may present with paraparesis.
- **Infections:** Some infections affecting the spinal cord, such as certain viral or bacterial infections, can cause paraparesis.
- **Vascular Issues:** Reduced blood supply to the spinal cord, as seen in conditions like spinal cord infarction, may result in paraparesis.
3. **Clinical Presentation:**
- **Weakness:** Gradual or sudden onset weakness in both legs.
- **Difficulty Walking:** Individuals with paraparesis may have difficulty walking, maintaining balance, or coordinating leg movements.
- **Sensory Changes:** In addition to weakness, there may be sensory changes, such as numbness or tingling, in the affected areas.
4. **Diagnosis:**
- **Neurological Examination:** A healthcare provider will conduct a thorough neurological examination to assess muscle strength, reflexes, and sensory function.
- **Imaging Studies:** Magnetic Resonance Imaging (MRI) or Computed Tomography (CT) scans may be used to visualize the spinal cord and identify potential causes.
- **Blood Tests:** Blood tests may be performed to check for infections or systemic conditions that could contribute to paraparesis.
5. **Treatment:**
- **Underlying Cause:** Treatment is often directed at addressing the underlying cause. This may involve surgery, medications, physical therapy, or a combination of approaches.
- **Rehabilitation:** Physical therapy and rehabilitation play a crucial role in managing paraparesis, aiming to improve mobility, strength, and overall function.
The management of paraparesis is individualized based on the underlying condition and the specific symptoms presented by the individual. Early diagnosis and intervention are essential for optimizing outcomes and improving the individual's quality of life. If someone is experiencing symptoms of paraparesis, seeking prompt medical attention for a thorough evaluation is important.
• Fixed flexion deformity ?
Fixed flexion deformity refers to a condition in which a joint, typically a knee or elbow, is permanently bent or flexed, and cannot be straightened to its normal range of motion. This deformity can result from various underlying causes, and it may affect one or more joints. Here are some key points about fixed flexion deformity:
1. **Causes:**
- **Muscular Imbalance:** Imbalance between the muscles that flex and extend the joint can lead to a fixed flexion deformity.
- **Joint Contracture:** Conditions such as joint inflammation, trauma, or prolonged immobility can cause contracture of the joint capsule or surrounding tissues, limiting movement.
2. **Common Sites:**
- **Knee:** Fixed flexion deformity of the knee is often associated with conditions like osteoarthritis, rheumatoid arthritis, or post-traumatic injuries.
- **Elbow:** Conditions such as elbow contracture, often seen after fractures or dislocations, can result in fixed flexion deformity.
3. **Clinical Presentation:**
- **Limited Range of Motion:** The affected joint cannot be fully extended or straightened.
- **Functional Impairment:** Difficulty with walking, weight-bearing, or performing activities that require a full range of motion.
4. **Diagnosis:**
- **Physical Examination:** A healthcare provider will assess the affected joint's range of motion and may identify any contractures or deformities.
- **Imaging Studies:** X-rays or other imaging modalities may be used to evaluate the joint structure and identify any underlying conditions.
5. **Treatment:**
- **Physical Therapy:** Stretching exercises and physical therapy may help improve joint flexibility and prevent further contracture.
- **Orthotic Devices:** Braces or splints may be used to maintain joint alignment and prevent further deformity.
- **Surgical Interventions:** In severe cases, surgical procedures may be considered to release joint contractures or correct underlying structural issues.
6. **Underlying Conditions:**
- **Arthritis:** Inflammatory or degenerative arthritis can contribute to joint deformities.
- **Trauma:** Joint injuries, fractures, or dislocations can result in fixed flexion deformity.
- **Neurological Conditions:** Certain neurological disorders may lead to muscle imbalances and joint contractures.
Management of fixed flexion deformity often involves addressing the underlying cause, along with physical therapy and, in some cases, surgical interventions. Early diagnosis and intervention are essential for better outcomes. Individuals experiencing joint stiffness or deformity should consult with a healthcare professional for a thorough evaluation and appropriate management.
• Orthopnea Heart failure in CKD ?
Learning points
• How to approach an uncooperative patient ?
• How to make out Differential diagnosis by chief complaints ?
• Importance of series of events of patient from where he was absolutely alright
• Head to toe examintion and gait itself gives us CNS diagnosis
• Drug doses and treatment






Comments
Post a Comment